Dermatology in Asians (For Professionals)
1. Asians: who are they ?
-they represent 4.5% of population of the US.
-they are the people who come from the Far-east, South-East Asia and the Indian subcontinent.
-Standards of beauty are different than in the West but very diverse as very different cultures live there (light skin is sought after but unregulated stores must be avoided). The same goes for alternative medicine
2.Pigmentation disorders
a. Melasma:
-Affects women and 10% of men. This represents 5-6million people in the US who are mostly Asians and Hispanics.
-Causes are: genetic, ultraviolet light, pregnancy, hormonal treatments (oral contraceptive pill…) but the exact etiology is unknown. It associated with thyroid disorders.
-There are 2 clinical types: centrofacial or malar
-Woods light enables determination of the level of pigment:
- superficial (enhancement of color)
- deep (no enhancement of color)
- mixed
- indeterminate (type VI and dense pigmentation)
-Look for subclinical melasma ! (1/4 of patients). This is important as more superficial pigment will respond better to treatments whereas deeper located pigment will respond with more difficulty and will require methods such as lasers.
-Differential Diagnosis: Acquired bilateral nevus of Ota (Hori’s nevus), Ochronosis, Riehl’s melanosis (pigmented contact dermatitis), Pigmented Actinic Lichen Planus
-Progresses in research
- KANG 2002. Study in Korean patients: increased number of melanocytes
- KIM EH 2007: increase vascularity in lesional skin (vessel size density and area)
b. Post-Inflammatory Hyperpigmentation
-secondary to many diseases (Acne, Eczema, Psoriasis, Seborrheic Dermatitis, Lichen Planus)
-pigmentation can be epidermal or dermal: utility of wood’s lamp
-Treatment (also for melasma):
-sun protection
-treat and avoid triggers
-simplify skin care (lots of products in traditional shops are unregulated and can be contaminated with substances sometimes dangerous such as mercury)
-reduce pigmentation:
-DRUGS:
- HYDROQUINONE (twice a day on affected areas, 2-4% concentrations, 5-10% available, store in refrigerator, highly reactive oxidant and inefficacious when turns brown + stabilization of product by forming a compound with with ascorbic acid, side effects: ICD (irritant contact dermatitis) and ACD (allergic contact dermatitis), nail discoloration, halo hypopigmentation, conjonctival melanosis, exogenous ochronosis (the later is actually rare in asians Tan IJD 2008)
- AZELAIC ACID: available in concentrations of 15% gel or 20% cream, has no effect on normal skin, solar lentigines and freckles, takes months to work.
- ARBUTIN: risk of paradoxical hyperpigmentation if high concentration, 3% in Japan
- KOJIC ACID: fungal derivative, as efficacious as 2% hydroquinone, The principal side effect is contact dermatitis. Available in 2-4% concentrations.
- …Compounds (tretinoin, steroid, hydroquinone, ascorbic acid, salicyclic acid…) are also available and the best is to determine formulations with a pharmacist. To learn more about another effective depigmenting cream, click here.
-NON DRUG TREATMENT (Resurfacing: Chemical Peels, IPL, Microdermabrasion, Lasers when the pigment is deeper:
- Chemical Peels:
- Alpha hydroxyacids: causes keratolysis and desquamation. Must be neutralized within 2-4 minutes
- Beta Hydroxyacids: salicylic acid, self-neutralizing, comedolytic (acne) and keratolytic.
- Comment: peelings in Asians should remain epidermal (superficial). Retinoids should be stopped one week before the treatment and the area should be pretreated with hydroquinone for 4 weeks, 4-6 weeks interval between treatments
- Lasers/ lights:
-ablative lasers make the pigmentation worse
-Q-Switched lasers and Intense pulsed lights (IPL) carry mixed results (For melasma: Negishi 2004: actually worsening of pigmentation in this study
-transient improvement with fractional lasers (For melasma: Hyoun SL , 2009)
-importance of performing test spots
-time and patience !
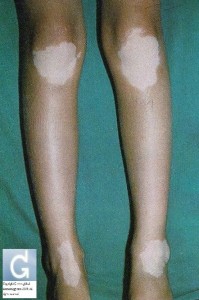
c. Vitiligo
-epidemiology: affects 1% US (0.1-2% worldwide), men and women equally affected, onset at any age but peaks at ages 10-30 yo
-affected areas: face, joints, hands, legs most common
-associated with endocrinopathies mostly thyroid auto-immune disorders (TSH dosage)
-causes include a genetic background (immediate family members are 5 times more likely to be affected whereas extended family members are 3 times more likely to be affected). The actual pathophysiology is truly unknown
-types: focal, segmental (associated poliosis), acrofacial (if fingertips involved depigmentation recommended as difficult to treat), generalized (vitiligo vulgaris), universal
-proven treatments: sun avoidance, camouflage, topical steroids, topical immunomodulators, systemic steroids, excimer laser (308nm), phototherapy (response should be seen 4-8 weeks), grafting, depigmentation (20% monobenzyl hydroquinone: acts by indices melanocyte death, takes 6-12 months to work, BSA (Body Surface Area involved) must be more than 50%, psychiatry assessment is needed, side effects include: Allergic contact dermatitis (ACD), consort vitiligo (persons in close contact persons catch vitiligo)…requires lifelong photoprotection, maintenance treatment (pharmacy in Tampa FL (1-8002267094, 31USD for 30g tube)), autologous melanocyte transplant (only 10% of donor surface is needed to fill recipient zone) (periorficial locations respond less efficiently to treatment).
-repigmentation patterns: perfollicular (most common), marginal (best response), diffuse, combined
surgical repigmentation is warranted when other therapies fail (immunomodulators, steroids, phototherapy). Stable for 6 months (ideally 12 months)
3.Acne Vulgaris
-more commonly inflammatory
-PIH and scarring common complaints. The most important is to prevent worsening of pigmentation by using sunprotection and avoiding the sun as much as possible.
-delayed presentation (go see doctors when alternatives have been tried)
-Treatments: Benzoyle Peroxyde (BPO(2.5-5%): can be combined with antibiotics (AB) (clindamycin, erythromycin), sulfur, azelaic acid (for PIH), topical retinoids (higher risk of irritancy), oral AB (oral cyclines, doxycycline preferred, if risk of PIH use doxycycline longer at dosage of 50mg once a day), spironolactone (start at 50mg and increase to 50mg twice a day (dosage of potassium and creatinine after one month), isotretinoin (1mg/kg/j), salicylic acid chemical peels, fractionated laser (442.5MHZ, less passes but more treatments)
4.Uncommon Diseases (but more frequent in Asians)
Erythema Dyschromicum Perstans (Ashy Dermatosis) (Bloch Sulzberger disease)
Progressive Macular Hypomelanosis (PMH): associated sometimes with Tinea Versicolor. Treatments like acne vulgaris
5 Malignant Melanoma
-It is rare: 1 in 100000
-Incidence peaks at age 60
-Types are mostly acral lentiginous melanoma. Superficial spreading the most common histological type. Survival rates are much higher (at least in the US).
-Prevention: The most important is to create skin cancer awareness (Asians do not even think about the risk).
6 Ethnic practices
-Often mimicks abuse
-TCM (Acupuncture, Cupping, Moxibustion, Coining (Spooning) (Vietnam) (rub on the back)
-Hair oils (especially in India) (strong dermatophyte efftect)
- mustard oil
- coconut oil
-Henna (Hair dye and painting of hands) (For black henna: contact dermatitis and permanent scarring)
-Sari and petticoat drawings
-vitiligo
-scarring
-Squamous Cell Carcinoma (SCC)
-Bindi (Tilak, Teep): Contact dermatitis
-Threading (hair removal method in India)
Contributors:
Dr Christophe HSU – dermatologist. Geneva, Switzerland
Source of information: Dermatologic Disease in Asians, Kundu R. 69th Annual Meeting of the AAD (American Academy of Dermatology) – New Orleans, Louisiana, United States of America (USA).
Category : Acne Vulgaris - Modifie le 03.25.2011Category : acne vulgaris - Modifie le 03.25.2011Category : asians - Modifie le 03.25.2011Category : asiatiques - Modifie le 03.25.2011Category : chloasma - Modifie le 03.25.2011Category : Dermatologie chez les asiatiques - Modifie le 03.25.2011Category : Dermatology in Asians - Modifie le 03.25.2011Category : hyperpigmentation post-inflammatoire - Modifie le 03.25.2011Category : masque de grossesse - Modifie le 03.25.2011Category : melanoma - Modifie le 03.25.2011Category : mélanome - Modifie le 03.25.2011Category : melasma - Modifie le 03.25.2011Category : post-inflammatory hyperpigmentation - Modifie le 03.25.2011Category : pregnancy mask - Modifie le 03.25.2011Category : vitligo - Modifie le 03.25.2011