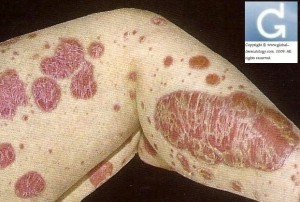
Plaque Psoriasis (for professionals)
- Psoriasis is a frequent inflammatory dermatosis which affects 1 to 2% of the global population. It is more frequent in Scandinavia and Europe. It is less frequent in Blacks and Chinese and is a rarity in Ethnic American-Indian population.
- Its cause is genetic (PSOR1 gene on chromosome 6) and environmental (guttate psoriasis for example has a specific infectious etiology (streptococcal pharyngitis)).
Algorythm
Limited psoriasis (less than 20% of the body surface area)
- topical steroids +/- vitamin D analogues (calcipotriene or calcitriol). No more than 100g per week of the latter because of hypercalcaemia induction (this represents 14g per day of 56% of the body surface area)(1g of cream treats an equivalent of 4% of the body surface area).
- intralesional steroids
- coal tar: these can be used in combination with topical corticosteroids. No conclusive study exists which would suggest that the theoretical risk of skin cancer due to usage of this agent.
- anthralin: it is derived from chrysarobine. It is often useful when applied daily for short periods. It is nevertheless irritant and can stain clothes and tiles. It can be combined with phototherapy (Ingram regimen).
- retinoids: tazarotene
Phototherapy
- Narrow Band UVB (311nm): start at 70% of the minimal erythemal dose. Increase weekly 10-30%. 3 to 5 sessions per week. Remission is usually achieved after 1 to 1 and a half months.
- PUVA or topical PUVA: after oral intake or topical application of a psoralen. Dosage varies according to the phototype.
- Multiclear (localised UVA and UVB treatment).
“Classical” systemic treatments
- retinoids (acitretin)
- methotrexate (7.5-25mg per week) to associate with folic acid (1mg/d)
- ciclosporine (3-5mg/Kg/d)
- fumaric acid (according to progressive dosage guidelines)
“Additional” systemic treatments
- apremilast (30mg bd)
“biologic” systemic treatments
- Indications:
- no response to classical systemic treatments have been seen or their usage is contraindicated.
- the PASI (Psoriasis Area Severity Index) of at least 15.
Short term response rates
–adalimumab:
- 70% of treated individuals achieve an improvement of PASI 70
- 45% of treated individuals achieve an improvement of PASI 90
- in both cases, the dosage is of 40mg every 2 weeks, after an induction dosa of 80mg
–etanercept:
- 35% of treated individuals achieve an improvement of PASI 70 and 10% have an improvement of PASI 90 after a dosage of 2 times 25mg per week.
- 50% of treated individuals achieve an improvement of PASI 70 and 20% have an improvemnet of PASI 90 after a dosage of 2 times 50mg per week.
–infliximab: for a dosage of 0.5mg/Kg at weeks 2, 4 and 6
- 80% of treated individuals achieve an improvement of PASI 70.
- 40% of treated individuals achieve an improvement of PASI 90.
–ustekimumab: for a dosage of 45mg every three months:
- 70% of treated individuals achieve an improvement of PASI 70.
- 40% of treated individuals achieve an improvement of PASI 90.
- To summarize, infliximab achieves the fastest results but it requires an intravenous infusion every 6 weeks.
- With ustekimumab, the improvement of PASI 90 is maintained 76 weeks after initiation of treatment in 63% of patients at a dosage of 90mg and in 45% of patients at a dosage of 45mg.
- Adalimumab also remains efficient 2 years after initiation of treatment.
- How to start a biologic ?:
- why start it: it must not have responded to other systemic agents, the severity of PASI must be at least 15.
- which one to chose: adalimumab (anti-TNF), infliximab (anti-TNF), etanercept (anti-TNF)m, ustekimumab (anti IL-12): no real guidelines exist. Personal experience is therefore a must.
- Therapeutic advice according to the histological caracteristics (proven or suspected)
- keratolytics for hyperkeratosis
- 2-5% salicylic acid (up to 20% concentration in palmar and plantar locations)
- emollients for parakeratosis
- anthralin, topical steroids, vitamin D analogues and phototherapy for psoriasiform hyperplasia
- topical steroids, cyclosporin, fumaric acid and biologics for erythema.
This advice is for informational purposes only and does not replace therapeutic judgement done by a skin doctor
Bibliography
Dermatology Secrets, 3rd edition, Mosby-Elsevier
Dermatology, 1st edition, Thieme
Notes on HMDP visiting expert Prof JH Saurat conference.
Category : plaque type psoriasis - Modifie le 09.14.2010Category : psoriasis en plaques - Modifie le 09.14.2010Category : traitement - Modifie le 09.14.2010Category : traitements - Modifie le 09.14.2010Category : treatment - Modifie le 09.14.2010Category : treatments - Modifie le 09.14.2010